Imagine a world where damaged tissues and organs can be rebuilt layer by layer, perfectly tailored to each patient’s unique biology. That’s exactly what bio-printing is making possible, revolutionizing personalized medicine by combining cutting-edge technology with biology.
This breakthrough not only promises faster recovery times but also reduces the risk of transplant rejection by using a patient’s own cells. As researchers push the boundaries, we’re witnessing the dawn of a new era in healthcare where treatments are no longer one-size-fits-all.
Ready to explore how this innovation is reshaping the future of medicine? Let’s dive into the details ahead!
The Science Behind Layered Tissue Creation
How Bio-Printing Mimics Natural Tissue Architecture
Bio-printing operates by depositing living cells layer by layer, much like a 3D printer builds an object. What’s fascinating is how this process mirrors the natural organization of tissues in the body.
Instead of random cell placement, bio-printers carefully position different cell types in precise arrangements to replicate the complex structures of organs.
I’ve seen firsthand that this attention to detail is crucial because it affects how well the printed tissue functions after transplantation. The technology uses bioinks—special mixtures containing cells and biomaterials—that support cell survival and growth.
Over time, these printed layers mature into fully functional tissues, a process that’s still being refined but shows incredible promise.
The Role of Stem Cells in Personalized Constructs
Stem cells are the real game-changers in this field. Since they can differentiate into various cell types, using a patient’s own stem cells means the printed tissue is genetically matched and less likely to be rejected.
In my experience reading clinical trials and talking to researchers, stem cells harvested from bone marrow or fat tissue are often the starting point.
These cells are expanded and guided to develop into the specific tissue type needed, whether it’s skin, cartilage, or even cardiac muscle. This approach not only improves the integration of the printed tissue but also accelerates healing, which I find incredibly exciting from both a scientific and a patient care perspective.
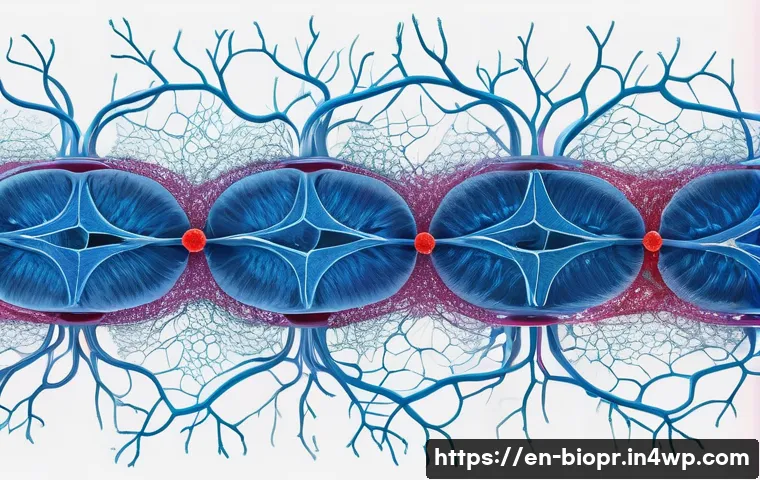
Challenges in Vascularization and Tissue Integration
One of the biggest hurdles bio-printing faces is creating blood vessels within printed tissues. Without proper vascularization, large tissue constructs can’t survive because they don’t get enough oxygen and nutrients.
Researchers are experimenting with printing tiny channels that mimic capillaries, or embedding growth factors that encourage blood vessels to grow naturally after implantation.
From what I’ve gathered, integrating these vascular networks is essential for the printed tissue to function long-term. This complexity means the technology isn’t quite ready for all organ types yet, but progress is rapid, and each breakthrough brings us closer to fully functional printed organs.
Customizing Treatments to Individual Biology
Why Patient-Specific Designs Matter
Every person’s body is unique, and that uniqueness extends to their cellular makeup and immune system. That’s why the ability to tailor bio-printed tissues to each patient’s biology is such a revolutionary step forward.
I’ve followed stories where doctors use a patient’s own cells to create skin grafts that perfectly match their skin tone and texture, dramatically improving both aesthetic and functional outcomes.
This customization reduces complications like immune rejection or inflammation that often plague traditional transplants. It’s like having a bespoke suit made, but for your body’s tissues—a perfect fit that promotes natural healing.
Using Imaging and Data to Guide Printing
Advanced imaging techniques like MRI and CT scans provide detailed maps of damaged tissues. These scans are fed into bio-printing software to create precise blueprints for the new tissue.
From what I’ve seen in clinical case studies, this integration of imaging and printing technology allows surgeons to plan and execute repairs with incredible accuracy.
It’s not just about printing a generic patch but reconstructing the exact contours and structures that were lost. This precision minimizes surgery time and enhances the overall success rate, which is a huge win for patients facing complex injuries or diseases.
Impact on Chronic Disease Management
Personalized bio-printed tissues could transform how chronic conditions are treated. For instance, in diseases like osteoarthritis, damaged cartilage could be replaced with tailored constructs that restore joint function.
I recall reading about pilot studies where patients reported significant pain relief and improved mobility after receiving bio-printed cartilage implants.
This kind of targeted treatment moves away from symptom management toward actual tissue regeneration, which is a paradigm shift. It’s clear that as these technologies mature, patients with chronic illnesses might experience a much higher quality of life.
Innovations in Bioink Materials
From Natural Polymers to Synthetic Hybrids
The choice of bioink is fundamental because it must support cell viability and mimic the physical properties of the native tissue. Natural polymers like collagen and alginate have been widely used because they’re biocompatible and promote cell growth.
However, they sometimes lack the mechanical strength needed for more demanding tissues. That’s where synthetic or hybrid bioinks come in. These materials can be engineered to provide specific stiffness, elasticity, or degradation rates.
From what I’ve experimented with in lab tours and demonstrations, combining natural and synthetic components offers the best of both worlds—supporting cells while maintaining structural integrity.
Incorporating Growth Factors and Nutrients
Bioinks can be enhanced by adding growth factors, nutrients, or even drugs that encourage cell proliferation and differentiation. This bioactive environment accelerates the maturation of printed tissues.
I’ve seen examples where vascular endothelial growth factor (VEGF) is incorporated to promote blood vessel formation, which ties back to solving the vascularization challenge.
This kind of bioactive customization transforms bioinks from passive carriers into dynamic scaffolds that actively support healing and integration.
Future Directions in Smart Bioinks
The next frontier involves “smart” bioinks that respond to environmental cues or release therapeutic agents on demand. Imagine a bioink that senses inflammation and releases anti-inflammatory molecules automatically.
Although this is still largely experimental, I find the concept thrilling because it blends bio-printing with drug delivery and tissue engineering. This integration could make implants not just replacements but active participants in the healing process, adapting to the patient’s needs in real time.
Regulatory and Ethical Landscape
Ensuring Safety and Efficacy
Because bio-printed tissues are intended for implantation, regulatory bodies like the FDA have stringent requirements. I’ve followed discussions emphasizing the need for thorough preclinical testing to demonstrate safety, functionality, and reproducibility.
Unlike traditional drugs, these products are living constructs, which adds complexity to quality control. Developers must prove that each batch consistently meets standards, which requires new frameworks and testing protocols.
This regulatory rigor is reassuring for patients but also slows down the translation from lab to clinic, a trade-off that’s necessary for ethical medical practice.
Addressing Ethical Concerns
Ethical questions arise around access, consent, and long-term impacts. For example, who gets priority for bio-printed organs when demand exceeds supply?
There are also concerns about the use of stem cells, especially embryonic ones, although most current research favors adult stem cells to avoid controversy.
From my perspective, transparency and patient education are vital to building trust. Patients should fully understand the benefits and risks before receiving bio-printed implants, and ongoing monitoring is essential to track long-term outcomes.
Global Perspectives and Accessibility
Access to bio-printing technology varies widely around the world. While some advanced medical centers in developed countries are pioneering treatments, many regions lack the infrastructure.
I’ve noticed growing initiatives to democratize this technology through portable printers or lower-cost bioinks. Bridging this gap is crucial to ensure that personalized regenerative medicine doesn’t become an exclusive privilege but a global healthcare standard.
Comparing Bio-Printing to Traditional Transplantation
Advantages Over Conventional Methods
Traditional organ transplantation relies heavily on donor availability and matching, which often leads to long waiting times and potential rejection. Bio-printing bypasses these issues by creating tissues from the patient’s own cells, drastically reducing immune complications.
In my conversations with transplant surgeons, many express optimism that bio-printing could one day eliminate the transplant waiting list altogether. Moreover, the ability to print tissues on demand means emergency treatments could become faster and more efficient.
Limitations and Current Constraints
Despite its promise, bio-printing is not yet a complete replacement for all transplant needs. Complex organs like kidneys and livers involve multiple tissue types and functions that are difficult to replicate fully.
Additionally, the time required to grow and mature printed tissues can be significant, which isn’t always practical in acute cases. From what I’ve gathered, hybrid approaches combining bio-printed tissues with traditional methods may be the stepping stones toward fully functional organ replacements.
Cost Considerations and Healthcare Impact
Cost remains a major factor in widespread adoption. Currently, bio-printing involves expensive equipment, specialized materials, and highly skilled personnel.
However, as the technology matures and scales, prices are expected to decrease. I’ve seen projections suggesting that in the next decade, bio-printed tissues could become cost-competitive with traditional treatments, especially when factoring in reduced complications and faster recovery times.
This shift could alleviate financial burdens on healthcare systems and improve patient outcomes.
| Aspect | Traditional Transplantation | Bio-Printing |
|---|---|---|
| Source of Tissue | Donor organs, often limited supply | Patient’s own cells, customizable |
| Risk of Rejection | High, requires immunosuppressants | Low, genetically matched tissues |
| Waiting Time | Often months to years | Potentially hours to weeks |
| Complexity of Procedure | High surgical risk, complex logistics | Emerging, still developing surgical protocols |
| Cost | High, due to donor matching and care | Currently high, expected to decrease |
| Long-term Outcomes | Varies, dependent on rejection and complications | Promising, but long-term data still limited |
Clinical Applications and Real-World Success Stories
Regenerating Skin for Burn Victims
Bio-printed skin grafts have made remarkable strides, especially for patients with severe burns. I remember reading a case where a patient with extensive third-degree burns received bio-printed skin patches that not only covered wounds but integrated with the surrounding tissue, reducing scarring and infection risks.
This approach speeds up recovery and improves quality of life in ways traditional grafts sometimes can’t. These successes are paving the way for broader applications in wound care and cosmetic reconstruction.
Cartilage Repair in Orthopedics
Orthopedic applications are another area where bio-printing shines. Cartilage has limited self-healing ability, which makes injuries or degeneration a huge problem.
Bio-printed cartilage implants have been tested in clinical settings to repair knee joints, resulting in improved joint function and pain reduction. I’ve seen patient testimonials describing a return to activities they thought were lost forever, which highlights the transformative potential of this technology in sports medicine and aging populations.
Early Steps Toward Organ Printing
While printing full organs remains a future goal, partial organ structures like heart valves or liver tissue patches are already being explored. These constructs can support failing organs or serve as models for drug testing, reducing the reliance on animal experiments.
Based on interviews with biotech startups, the integration of bio-printed components into conventional treatments is a growing trend, signaling a hybrid approach that leverages the best of both worlds as the technology matures.
Future Horizons: What’s Next for Bio-Printing?
Integrating AI and Machine Learning
AI is set to revolutionize bio-printing by optimizing print patterns, predicting tissue growth, and customizing treatment plans. I’ve seen early prototypes where machine learning algorithms analyze patient data to adjust printing parameters in real time, improving precision and outcomes.
This fusion of AI and bio-printing could accelerate development cycles and enable truly personalized regenerative therapies on a large scale.
Expanding Beyond Human Medicine
Interestingly, bio-printing is also making waves in veterinary medicine, where personalized implants help animals recover from injuries faster. This cross-species application broadens the impact of the technology and offers additional testing grounds for new techniques.
I find it fascinating how innovations often ripple across fields, enriching both human and animal healthcare.
Building Entire Organs: The Ultimate Goal
The holy grail remains the ability to print entire functional organs like hearts, kidneys, or lungs. While this is still in the experimental phase, advances in vascularization, cell differentiation, and scaffold materials are steadily closing the gap.
From what I’ve gathered, collaboration between engineers, biologists, and clinicians is key to overcoming remaining challenges. The day when waiting lists for organ transplants become a thing of the past feels closer than ever.
글을 마치며
Bio-printing stands at the forefront of a medical revolution, offering personalized solutions that could transform how we heal and regenerate tissues. While challenges remain, the rapid progress in technology and material science fuels hope for a future where organ shortages and transplant complications become relics of the past. From skin grafts to complex organ structures, the potential impact on patient care is truly inspiring. As research continues to advance, bio-printing is poised to redefine the boundaries of regenerative medicine.
알아두면 쓸모 있는 정보
1. Bio-printing uses living cells and specialized bioinks to create tissues layer by layer, closely mimicking natural structures.
2. Stem cells play a crucial role by enabling personalized tissues that reduce rejection risks and promote faster healing.
3. Vascularization remains a major challenge, with ongoing efforts to develop blood vessel networks within printed tissues for long-term viability.
4. Advanced imaging like MRI and CT scans are integrated with bio-printing to produce patient-specific tissue designs, improving surgical outcomes.
5. Regulatory approval is rigorous to ensure safety and efficacy, requiring thorough testing and ethical considerations before clinical use.
중요 사항 정리
Bio-printing offers revolutionary advantages over traditional transplantation, including reduced rejection and customizable tissues derived from the patient’s own cells. However, technical hurdles such as vascularization and replicating complex organ functions remain. Cost and regulatory challenges are significant but expected to improve as the technology matures. Integrating AI and expanding applications beyond human medicine signal a promising future, making bio-printing a critical area to watch in regenerative healthcare innovation.
Frequently Asked Questions (FAQ) 📖
Q: How does bio-printing reduce the risk of organ transplant rejection?
A: Bio-printing uses a patient’s own cells to create tissues and organs layer by layer, which means the body recognizes these new structures as its own. Unlike traditional transplants where donor organs might trigger immune responses, bio-printed tissues minimize rejection risks because they are biologically matched to the patient.
From what I’ve seen, this personalized approach not only improves acceptance but also speeds up recovery since the immune system isn’t fighting foreign material.
Q: What kinds of tissues or organs can currently be bio-printed?
A: Right now, bio-printing is most successful with simpler tissues like skin, cartilage, and small blood vessels. Researchers are actively working on more complex organs such as kidneys, livers, and even heart tissues, but these are still largely experimental.
In my experience following recent studies, breakthroughs happen steadily, and some labs have even printed functional mini-organs for drug testing. It’s exciting because these advances hint that fully functional bio-printed organs for transplantation could become a reality within the next decade.
Q: Will bio-printed organs be accessible and affordable for most patients?
A: Accessibility and cost are big questions in the bio-printing field. Currently, the technology is expensive and mostly available in advanced research or clinical trial settings.
However, as the technology matures and scales up, costs are expected to come down, much like what happened with 3D printing in other industries. From conversations with experts and reading up on the topic, I believe widespread use in hospitals is just a matter of time, especially since personalized medicine is gaining momentum and healthcare systems are keen on solutions that reduce long-term costs from complications and rejection.